Abstract
Aim:
The prevalence of celiac disease in patients with iron deficiency (ID) in the United States is unknown. Estimating the prevalence of Celiac disease (CD) in patients with ID could help to determine the need to screen these patients for occult CD. In 2017, the United States Preventive Services Task Force stated that the current evidence is inadequate to assess the balance of benefits and harms of screening for CD in asymptomatic persons. Also, there are no current guidelines to advise physicians regarding the screening of patients with iron deficiency for occult CD.
Methods:
Data were obtained from the National Health and Nutrition Examination Survey (NHANES) database, a nationally representative health survey conducted from 2009 to 2010. We included 2,105 females aged 6 years or older. Iron deficiency was defined as serum ferritin level <20 ng/ml, and patients were considered positive for celiac disease when positive for both immunoglobulin A tissue transglutaminase antibody (IgA Ttga) and IgA endomysial antibody (IgA EMA). Subjects with Iron deficiency were divided into two groups (ID and Non-ID). The association of CD and ID, i.e., the primary outcome, was obtained after adjusting other covariates using logistic regression.
Results:
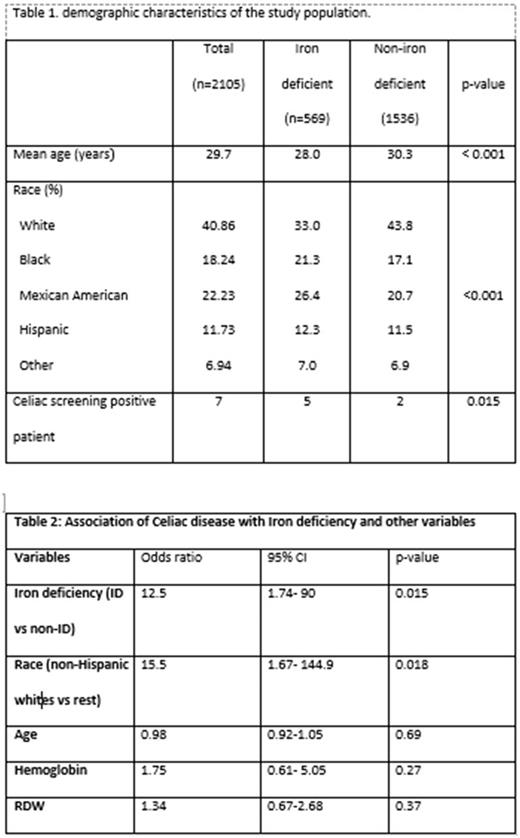
The mean age of our study population was 29.7 years; 28.0 years in the ID group and 30.3 in the non-ID group (p<0.001). Non-Hispanic whites constituted 41%of the total study sample. The demographic characteristics of the study population are shown in table 1.
There were 569 (27%) females who had ID and 1536 (73%) who did not have ID. The overall prevalence of CD in the study population was 0.33% (7/2105). The prevalence of CD in ID females was 0.9% (5/569), and the prevalence of CD in non-ID females was 0.1% (2/1536) with an odds ratio (OR) of 6.79 (95% confidence interval, 1.31-35.2). After adjusting for selected covariates, the prevalence of CD was higher in female subjects with ID with OR of 12.5 (95% CI 1.74-90). Although these results showed that CD did increase the risk of having ID in females, it did not show any difference in hemoglobin between celiac positive and celiac negative females with an odds ratio of 1.75 (95% CI 0.61-5.05).
Discussion
In this study, one in 113 iron-deficient females met the criteria for the diagnosis of occult CD compared to one in 676 non-iron deficient females. So, screening for occult CD could help in diagnosing the cause of ID and subsequently help in treatment. Celiac serology offers a non-invasive test to detect gluten hypersensitivity in females with ID. There is no study looking into the downside of screening for CD in asymptomatic people. However, potential disadvantages of CD screening may include increased anxiety, over-diagnosis, unnecessary serologic tests and increased need for unnecessary endoscopies with biopsy.
The strength of this study is that it includes a representative sample from a national database, which was adjusted for minority groups. However, this study also had several limitations. The number of cases of CD was very small due to the relatively low prevalence of CD in the United States (0.71%). Another limitation was our criteria for the diagnosis of CD based on serology only without histological confirmation, as a duodenal biopsy is an invasive test difficult to perform in a population-based study. However, this limitation is partially balanced by the sequential serological testing of IgA EMA in IgA tTGA positive individuals. Another potential limitation is that patients with IgA deficiency were missed by the study as IgA deficiency was not tested.
Conclusions:
Although the overall prevalence of celiac disease in the United States is low in the female population, the prevalence is higher in subjects with Iron deficiency. We suggest that CD testing should be considered in patients with refractory ID when other obvious causes have been ruled out. Further prospective studies are needed to validate this finding.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal